News Express: UM develops therapeutic approach for Parkinson’s disease using curcumin
新聞快訊:澳大研究團隊用薑黃素治療帕金森
NK細胞膜仿生薑黃素脂質體合成
Synthesis of NK cell membrane-camouflaged curcumin liposomes
澳大研究團隊用薑黃素治療帕金森
澳門大學健康科學學院教授袁振的研究團隊在帕金森疾病(PD)遞藥研究上取得重大進展。針對PD重大臨床需求,研究團隊通過細胞膜仿生工程技術構建一種 NK細胞膜包裹的中藥(薑黃素)脂質體新藥,以腦膜淋巴管(MLVs)作為藥物輸運通道,顯著提高帕金森症治療效率。該研究成果被國際知名期刊Research刊登。
PD是重大退行性腦疾病。當前,世界約有500萬PD患者,中國是世界上PD患者最多的國家,病例接近300萬。目前,PD治療以藥物為主,物理刺激為輔,前者受限於血腦屏障,後者是有創療法,且價格昂貴,適用人群有限。因此,發展高效的PD治療新方法和新技術,對維護人體健康、降低政府財政負擔和提高病人生活品質具有重要意義。
最新的腦疾病藥物干預研究表明,腦膜淋巴管是大腦最重要的中樞神經淋巴引流系統。2020年,中國學者首次採用腦膜淋巴管作為藥物輸運通道,成功繞過了血腦屏障的限制,將納米藥物遞送到腦組織,顯著提高了腦膠質瘤治療效率。但是腦膜淋巴管內有大量的記憶免疫細胞,如巨噬細胞、B細胞、T細胞等,它們發揮免疫監視作用,能快速清除納米藥物,降低藥物入腦效率。而且,藥物經腦膜淋巴管進入腦組織後,在全腦擴散,難以高效靶向病灶組織。因此,發展高效的以腦膜淋巴管為藥物遞送通道的方式,從而治療重大腦疾病仍面臨巨大挑戰。
該研究證明NK細胞膜仿生脂質體具有靶向受損神經元和抗免疫細胞吞噬的能力,並通過血腦屏障途徑高效入腦,顯著改善帕金森小鼠運動行為缺陷和病理損傷。另外,仿生脂質體可以抑制MPP+誘導的神經元凋亡和清除受損細胞分泌的α-syn 聚集體,從而防止更嚴重的神經元損傷。此外,它們可以消耗活性氧(ROS),對神經元產生神經保護作用。該研究不僅為仿生中成藥在帕金森症治療領域提供了新的契機,也為各種腦疾病治療提供了新的給藥思路。
是次研究的共同通訊作者為袁振和中國科學院深圳先進技術研究院研究員盛宗海,澳大博士生劉靜和博士畢業生高篤陽為共同第一作者。該研究獲澳門大學(檔案編號:MYRG2022-00054-FHS)資助。全文可瀏覽https://spj.science.org/doi/full/10.34133/research.0030。
欲瀏覽官網版可登入以下連結:
https://www.um.edu.mo/zh-hant/news-and-press-releases/campus-news/detail/55622/
UM develops therapeutic approach for Parkinson’s disease using curcumin
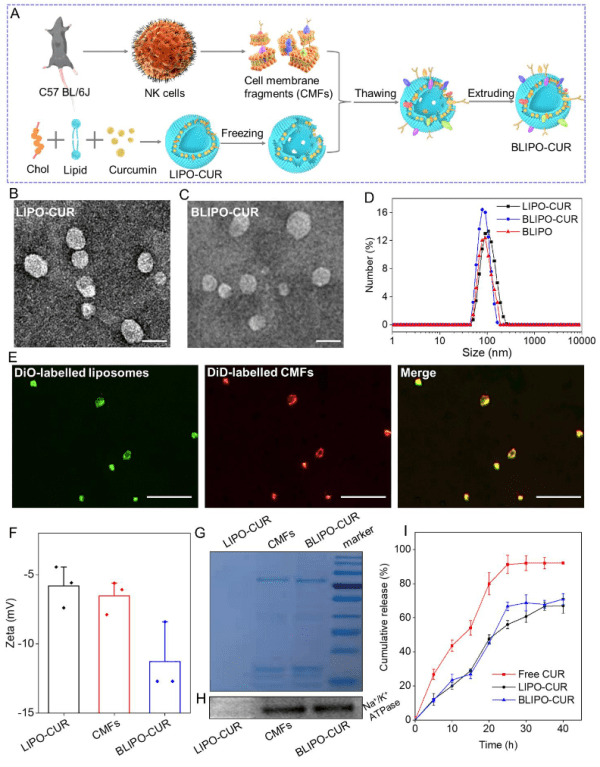
A research team led by Yuan Zhen, professor in the Faculty of Health Sciences (FHS) at the University of Macau (UM), has made a breakthrough in drug delivery for the therapy of Parkinson’s disease (PD). In response to a major clinical need for PD treatment, the team developed natural killer (NK) cell membrane-camouflaged curcumin (a traditional Chinese medicine) liposomes using cell membrane biomimetic technology. They also discovered that using meningeal lymphatic vessels (MLVs) as drug delivery routes could significantly improve the treatment efficacy of PD. The research results have been published in the internationally renowned journal Research.
PD is a major neurodegenerative disease. At present, about five million individuals are diagnosed with PD worldwide, and China has the largest number of PD patients in the world, with nearly three million cases. Current clinical treatments for PD mainly contain chemical drugs, supplemented with physical stimulation. The former is limited by the blood-brain barrier (BBB), whereas the latter is an invasive and expensive treatment with limited applicability to the population. Therefore, it is of great importance to actively develop new and efficient PD treatments for safeguarding health, reducing the financial burden on the government, and improving patients’ quality of life.
Recent studies on drug intervention in brain disorders have shown that MLVs are the most important component of the drainage system in the brain’s central nervous system. In 2020, Chinese researchers used MLVs as drug delivery routes for the first time, successfully bypassing the BBB to deliver nano-drugs to brain tissues, thereby significantly improving the efficiency of glioma treatment. However, MLVs contain large numbers of immune cells, such as macrophages, B cells, and T cells, which play an immune surveillance role and can quickly clear the nano-drugs, and reduce the efficiency of drug delivery to the brain. In addition, drugs delivered to the brain via the MLV route spread throughout the brain, making it difficult to efficiently target the lesion areas. Therefore, the development of an efficient drug delivery mechanism via MLVs for the treatment of severe brain diseases remains a major challenge.
In the study, NK cell membrane biomimetic liposomes demonstrated the ability to target damaged neurons, resist immune cell phagocytosis, and efficiently enter the brain via the MLV route, which significantly improved motor behaviour deficits and pathological damage in PD mice. In addition, biomimetic liposomes could inhibit MPP+-induced neuronal apoptosis and clear α-syn aggregates secreted by damaged cells, thus preventing more severe neuronal damage. Meanwhile, they could deplete reactive oxygen species (ROS) and exert a neuroprotective effect on neurons. The study not only offers new perspectives for biomimetic Chinese medicine for PD therapy, but also provides new ideas for drug delivery in the treatment of various brain disorders.
Prof Yuan and Shen Zonghai, a researcher at the Shenzhen Institute of Advanced Technology, Chinese Academy of Sciences, are the corresponding authors of the study. UM PhD student Liu Jing and PhD graduate Gao Duyang are the co-first authors. The project was funded by UM (File no: MYRG2022-00054-FHS). The full version of the research paper can be viewed at https://spj.science.org/doi/full/10.34133/research.0030.
To read the news on UM’s official website, please visit the following link:
https://www.um.edu.mo/news-and-press-releases/campus-news/detail/55622/